Consortium News
Welcome to the TRICIA News Page. Here you’ll find the latest updates from the Tissue Research in Childhood Inflammatory Arthritis (TRICIA) Consortium – including network updates, research discoveries, upcoming events, and stories from families and clinicians involved in our work to improve the future of children and young people with JIA.
Stay Connected with the TRICIA Network!
Be the first to hear about our latest research news. Whether you’re a researcher, clinician, patient partner, or supporter of paediatric rheumatology, sign up to receive updates and be part of the TRICIA community.
We promise not to overload your inbox—and you can unsubscribe at any time. Read the Privacy Notice
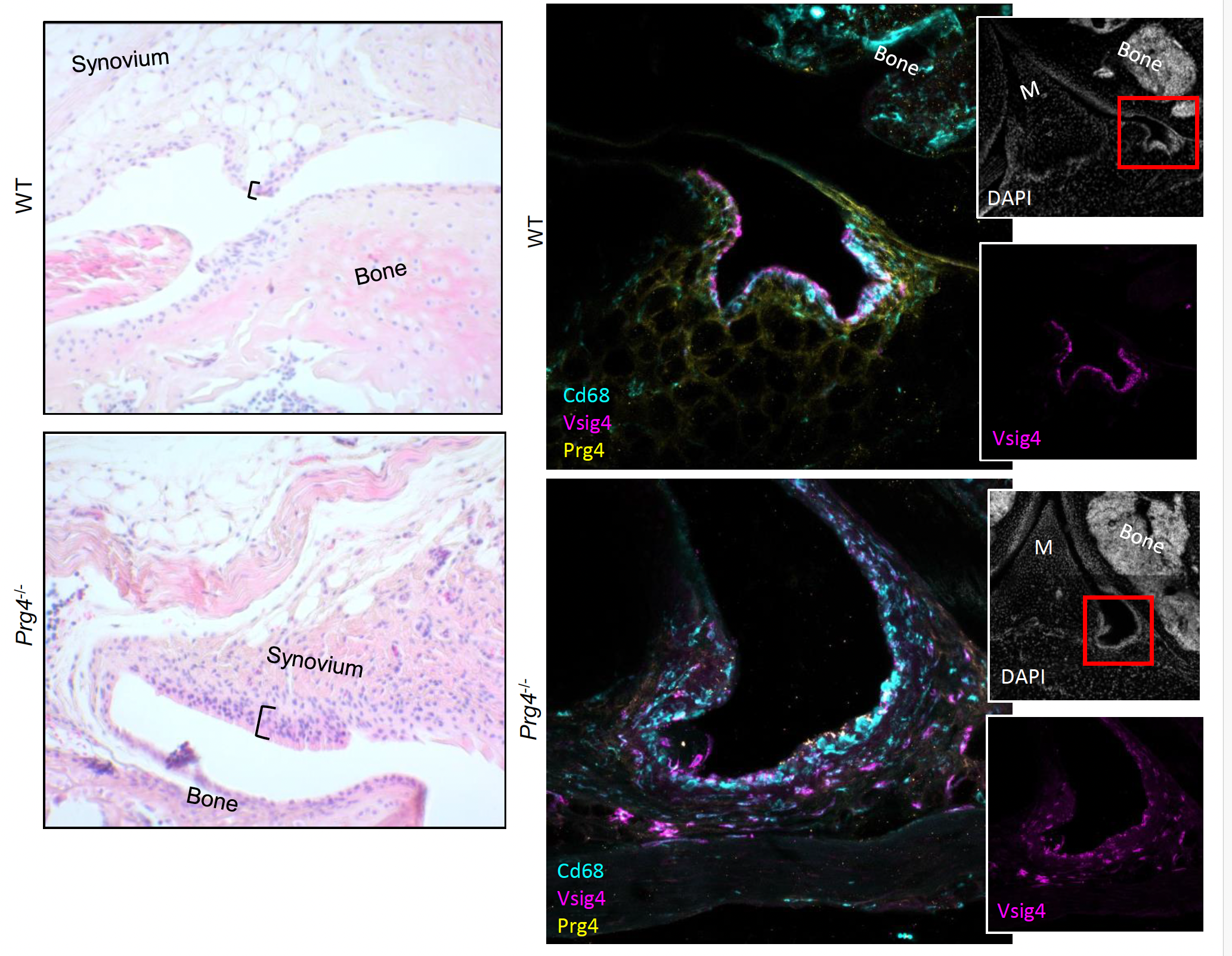
Defining Cellular Pathology in CACP Syndrome: A New Research Initiative
Exciting New Funding Award to Tackle Rare Childhood Arthritis Syndrome
Professor Adam Croft has received funding from Great Ormond Street Hospital Charity for a 3-year research project to study a rare genetic condition called Camptodactyly-Arthropathy-Coxa Vara-Pericarditis (CACP) syndrome.
This debilitating condition begins in early childhood, causing joint stiffness, swelling, and difficulty moving. It can also lead to fluid around the heart (pericarditis), impacting children’s daily lives. Currently, there is no cure or specific treatment.
Understanding the Cause
CACP syndrome is caused by changes in a gene called PRG4, which produces a protein called lubricin. Lubricin helps protect and lubricate joints. Without it, children experience painful joint damage and scarring. However, researchers still don’t fully understand why the lack of lubricin causes these symptoms.
This project will investigate how cells in the joint—called fibroblasts and macrophages—normally work together to keep joints healthy, and what goes wrong when lubricin is missing. The research team believes that without lubricin, macrophages can’t function properly, leading to overactive fibroblasts, inflammation, and scar tissue formation.
Who’s Involved?
Led by Prof. Croft at the University of Birmingham, the study brings together a team of experts from Birmingham Children’s Hospital and the UCL Great Ormond Street Institute of Child Health. It also uses precious joint tissue samples already collected through the UK-wide TRICIA (Tissue Research in Childhood Inflammatory Arthritis) network.
Guided by the Voices of Patients and Families
A unique feature of this study is how closely it has been co-developed with young people affected by CACP and their families. Through a series of meetings in spring 2024, young people (aged 13–21) and their parents shaped the study’s direction. Their experiences highlighted the urgent need to understand and treat joint contractures, which most impact daily life.
They also helped researchers decide when and how to collect tissue samples in an ethical and acceptable way, such as during clinical procedures already being done for care.
Families stressed the importance of new treatments and shared their views on side effects, educational impact, and participation in sports. Based on their input, the study now includes a dedicated work package focused on restoring lubricin and testing potential new therapies.
A National Research Effort
The project is part of the MRC-funded TRICIA consortium, which builds capacity for joint tissue research in children and young people across the UK. Samples used in this study were collected through MAPJAG, a TRICIA-linked study using safe, ultrasound-guided biopsies.
Ongoing Involvement and Communication
Three young people with CACP and their families will remain involved through a study advisory group, meeting regularly to guide research and ensure results are shared clearly and accessibly.
Dissemination will include lay summaries, social media updates, press releases, and public events. The study also contributes to training future scientists through the Patient Alliance initiative, where researchers are paired with PRPs to promote meaningful involvement throughout.

New Video – Amy’s Experience of Living with JIA
At the end of last year the MAPJAG research team collaborated with Amy, a young person living with Juvenile Idiopathic Arthritis (JIA), to create a new video highlighting the importance of research into the condition.
Showcasing the Patient Perspective The video, featuring Amy and Professor Adam Croft, Chief Investigator of MAPJAG, sheds light on the challenges of living with JIA and the vital role research plays in improving treatments. Amy shares her personal journey, including her diagnosis at age three, her experiences with different treatments, and how research has helped shape better understanding and care for young people like her. Professor Croft explains:“Through MAPJAG, we aim to better understand JIA and improve treatments for young people. Collaborating with Amy on this video has been invaluable in showing why research matters—not just to scientists and clinicians, but to the young people affected by this condition every day.”You can watch the video here: https://youtu.be/oXUB-dL2r_4. A Platform for Young Voices in Research Amy’s involvement in this video highlights the importance of patient engagement in research. By sharing her lived experience, she provides a powerful perspective on why studies like MAPJAG are essential for identifying better treatments and ensuring that young people receive the right support as early as possible. Amy reflects:
“It’s important that research focuses on the needs of young people with JIA. Being part of this video was a great opportunity to share my experience and to help raise awareness of the work being done to improve treatment options.”Expanding the Impact of MAPJAG The MAPJAG study continues to grow, supported by funding from the Kennedy Trust for Rheumatology Research, Versus Arthritis, the NIHR Birmingham Biomedical Research Centre, and the Medical Research Council, and remains committed to working closely with young people and their families. Through initiatives like this video, the research team hopes to increase awareness, encourage participation, and ensure that young voices remain at the heart of scientific progress.
New Video – The Importance of Research into JIA
Sharing the Patient Perspective
Two young people, Jasmine and Sophie, who both live with Juvenile Idiopathic Arthritis (JIA), have created a powerful video explaining why research into the condition is so important. As Patient Partner Group members, they contribute invaluable insights and feedback to the TRICIA network, ensuring that research reflects the real concerns of those living with JIA.
Why Research Matters
In the video, Jasmine and Sophie share their personal experiences with JIA, the challenges they face, and how research can improve treatment options. Their voices bring a unique and powerful perspective, helping researchers, funders, and other stakeholders understand the impact of JIA and the need for continued investment in research.
A Valuable Resource for Advocacy
The video serves as an impactful resource for presentations to funders, researchers, and healthcare professionals. Hearing directly from those affected by JIA reinforces the urgency of research and the real-life difference it makes. No one can articulate the need for progress better than those living with the condition.
Watch the Video
You can watch Jasmine and Sophie’s video here: https://www.youtube.com/watch?v=Io10pTLQlXY&t=21s
Produced in March 2024, this video is a testament to the importance of patient involvement in shaping research and driving meaningful change.

Nature Publication success for Chrissy Bolton
Congratulations to Dr. Chrissy Bolton, an MRC Clinical Research Training Fellow and paediatric doctor, on her recent publication in Nature Reviews Rheumatology titled “All fibroblasts are equal, but some are more equal than others.”
Dr. Bolton graduated from the University of Cambridge and UCL, earning national and university prizes in Paediatric Health, Endocrinology, Pain Medicine, Cardiology, and Ethics. She has contributed to pioneering studies on minimally invasive tissue biopsies in children with arthritis, collaborating with Professors Lucy Wedderburn and Adam Croft. Her research focuses on understanding inflammation persistence in juvenile idiopathic arthritis (JIA).
In her recent article, Dr. Bolton explores how epigenetic programming of synovial fibroblasts—the cells lining the joints—affects their response to inflammation. This research sheds light on why different joints may exhibit varying patterns of involvement and responses to treatment in arthritis.
This insight is significant for TRICIA’s mission to integrate synovial tissue analysis into clinical practice for JIA. Understanding the diverse behaviours of synovial fibroblasts can lead to more targeted and effective treatments for young patients with arthritis.
Read the full article >> Bolton, C., Croft, A.P. All fibroblasts are equal, but some are more equal than others. Nat Rev Rheumatol (2024). https://doi.org/10.1038/s41584-024-01097-6
Professor Adam Croft inaugural lecture: Restoring order to the joint: fibroblasts as cellular checkpoints of inflammation
On 6 March 2024, Professor Adam Croft, the Versus Arthritis Chair of Rheumatology and Head of the Rheumatology Research Group at the University of Birmingham, delivered his inaugural lecture titled “Restoring Order to the Joint: Fibroblasts as Cellular Checkpoints of Inflammation.”
In his lecture, Professor Croft explored the critical role of fibroblasts—structural cells within joint tissues—in orchestrating inflammation in chronic joint diseases such as rheumatoid arthritis. He described fibroblasts as the “conductors of the immunological orchestra,” highlighting their ability to either amplify or suppress inflammatory responses. His research has identified distinct fibroblast subtypes with specific functions: some contribute to joint damage, while others help regulate and resolve inflammation. This understanding paves the way for developing targeted therapies aimed at restoring joint health by modulating fibroblast activity.
The lecture was accessible both in person and online via Zoom, reflecting the university’s commitment to sharing knowledge widely. For those interested in a concise overview of Professor Croft’s insights, the University of Birmingham’s Marketing and Communications Team produced a video ahead of the lecture, available here: https://youtu.be/7pwe0jEzH2Q
Dr Chrissy Bolton – Runner-up in the GOSH Image Competition
Dr Chrissy Bolton, MRC Clinical Research Training Fellow and a valued member of the TRICIA team, was recently recognised as a runner-up in a prestigious research image competition. The competition, open to staff from Great Ormond Street Hospital (GOSH) and its affiliated institutes—the NIHR GOSH Biomedical Research Centre (BRC) and the UCL Great Ormond Street Institute of Child Health (UCL GOS ICH)—invited researchers to capture ‘a moment of discovery’ in their work.
This initiative also extended to other paediatric hospitals across the UK, including Alder Hey, Birmingham, and Sheffield, as part of the NIHR GOSH BRC Paediatric Excellence Initiative. From numerous entries, 11 shortlisted images and GIFs were reviewed by three independent panels: the GOSH Young People’s Advisory Group for Research (YPAG), NIHR GOSH BRC stakeholders, and GOSH staff networks. These images highlighted the groundbreaking research conducted across GOSH and its partner institutions, all striving to improve treatments for rare and complex childhood conditions.
Finalists were selected based on their impact and scientific significance, with the overall winner decided through a public vote on social media.
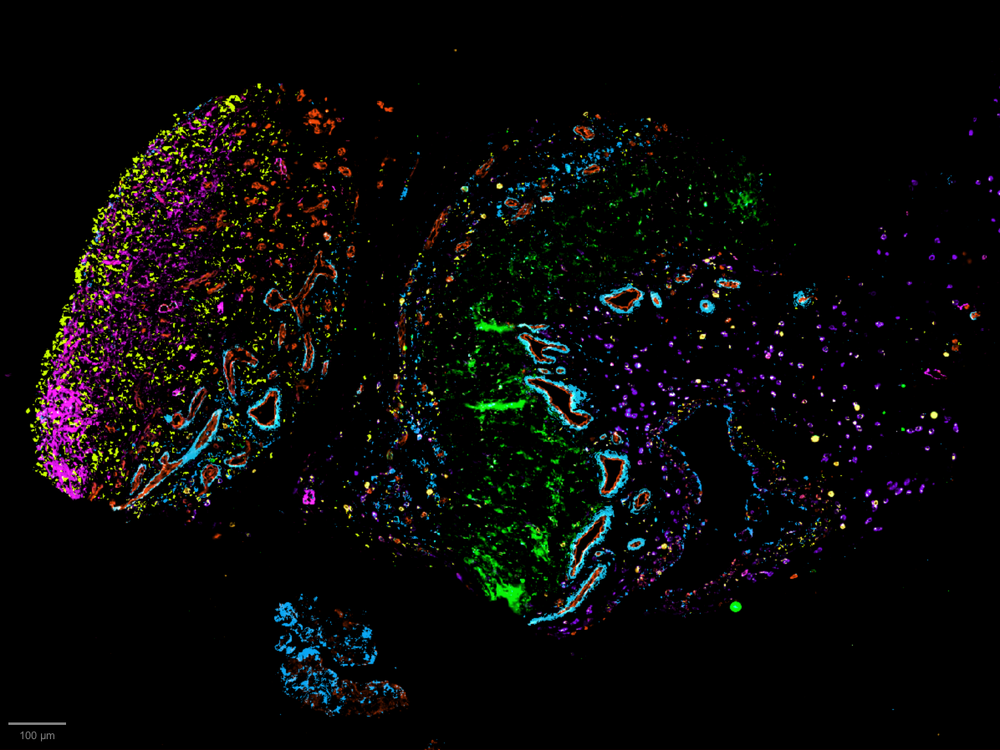
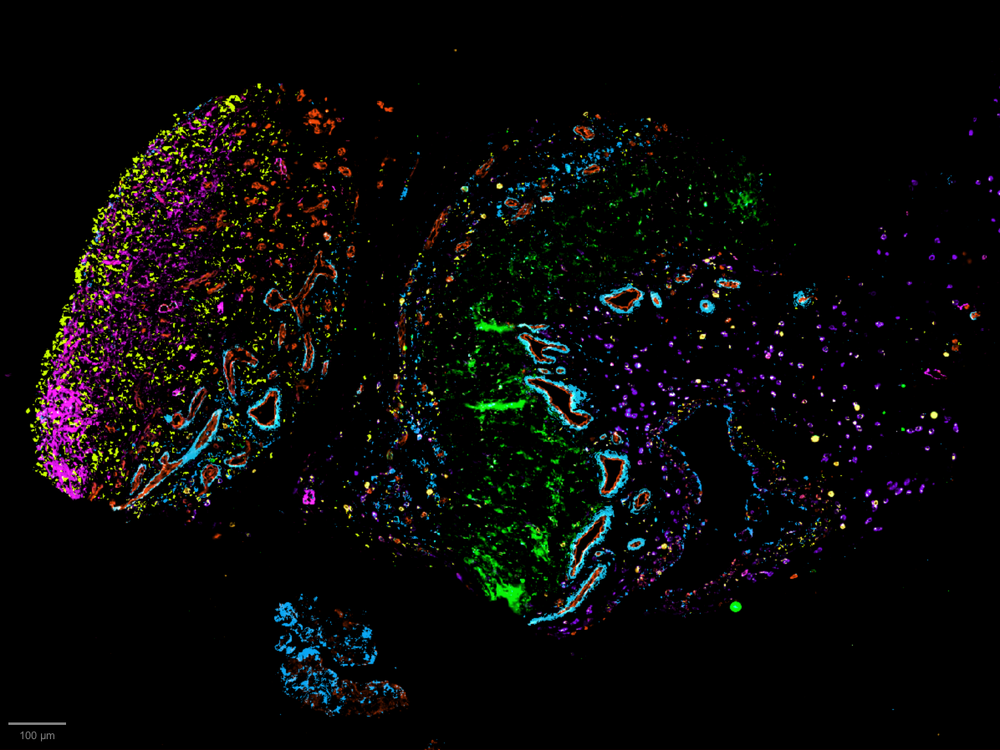
Capturing Childhood Arthritis: Chrissy Bolton’s Image
Dr Bolton’s submitted image provides a striking visual of the cellular landscape within the knee joint of a four-year-old child with arthritis.
• Blood vessels, shown in red, infiltrate the inflamed joint, signalling disease progression and attracting immune cells that drive tissue damage.
• The outer layers, depicted in yellow and pink, typically form a thin protective barrier but thicken as the joint reacts to ongoing inflammation.
• The green regions represent scar tissue, which contributes to joint stiffness and restricted movement.
In the UK, inflammatory arthritis affects approximately 1 in 1,000 children, most commonly impacting large jointssuch as the knees. Despite advancements in treatment, many children continue to experience persistent disease activity for over a decade. Historically, most arthritis research has focused on adults, leaving significant gaps in our understanding of how chronic inflammation develops in children’s immune systems.
This image serves as a powerful reminder of why paediatric-specific research is essential. Parents have been key advocates, demanding that their children benefit from the same cutting-edge scientific advancements as adults. Their voices underscore the urgent need for more research into childhood arthritis, ensuring better treatments and improved outcomes for young patients.

Emerging Investigator Excellence Awards by the American College of Rheumatology
Two researchers from the Institute of Inflammation and Ageing at the University of Birmingham, both affiliated with Professor Adam Croft’s research group and the TRICIA consortium, have been recognised with prestigious Emerging Investigator Excellence Awards by the American College of Rheumatology (ACR).
Dr Chris Mahony and Dr Sam Kemble received these competitive awards for their outstanding contributions to rheumatology research. The Emerging Investigator Excellence Awards acknowledge exceptional abstracts presented by early career researchers, with only one award granted per abstract category.
Dr Chris Mahony: Mapping the Inflamed Synovium in Childhood Arthritis
Dr Chris Mahony, a Postdoctoral Researcher, was recognised in the Paediatric Rheumatology – Basic Science category for his groundbreaking work on juvenile idiopathic arthritis (JIA). His research, titled:
🧬 “Cellular Deconstruction of Stromal and Myeloid Cell Compartments in the Inflamed Synovium of Juvenile Idiopathic Arthritis”,
has led to the creation of the first-ever atlas of the inflamed synovium in children with JIA. This landmark studyprovides new insights into the cellular mechanisms driving inflammation in JIA, paving the way for more effective, targeted treatments for children affected by the disease.
Dr Mahony’s research was made possible through funding from Versus Arthritis, the Kennedy Trust for Rheumatology Research, and the Medical Research Council (MRC).
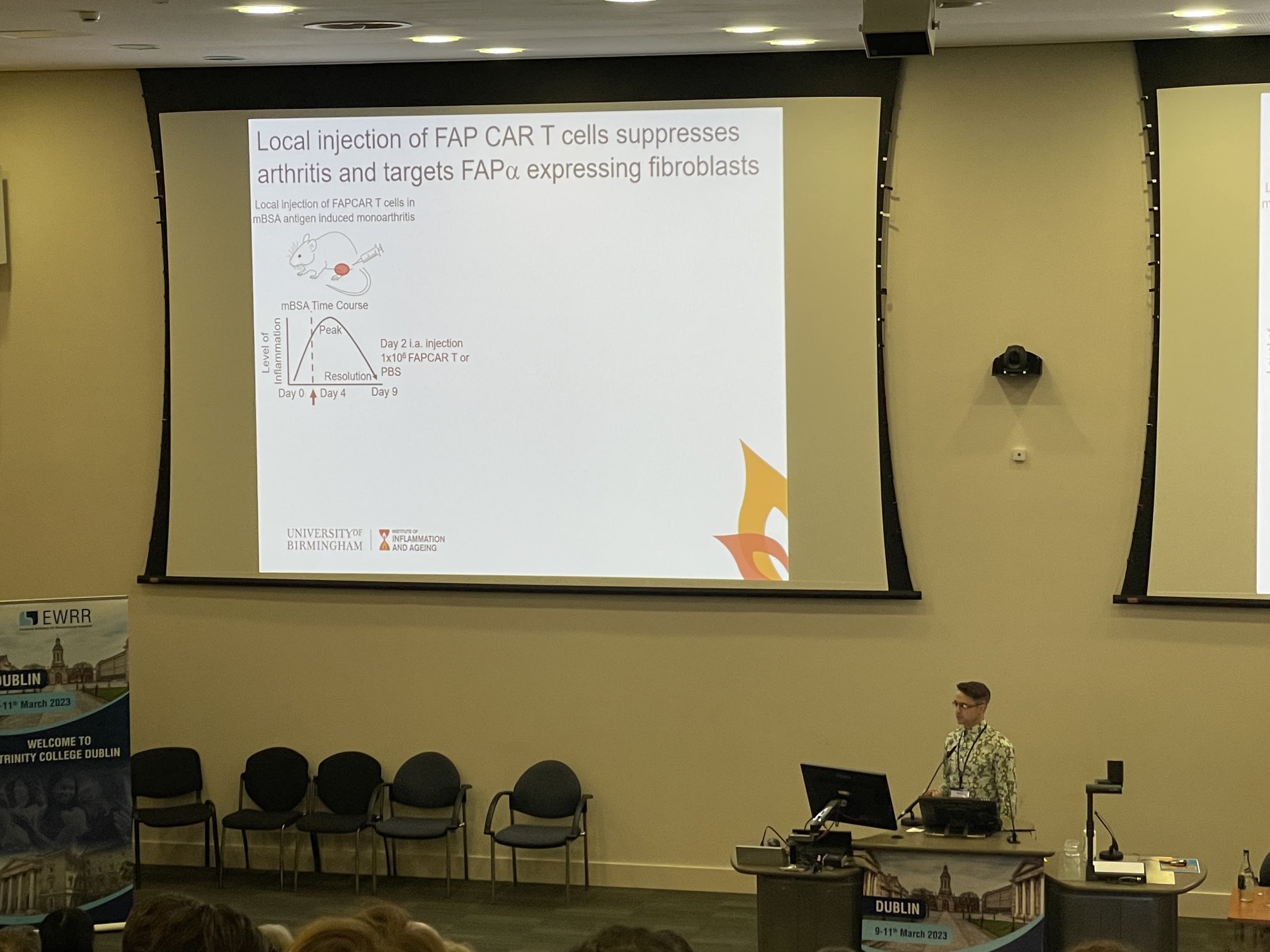
Dr Sam Kemble: Engineering T Cells to Target Fibroblasts in Inflammatory Disease
Dr Sam Kemble, a Research Fellow, was recognised in the T Cell Biology & Targets in Autoimmune & Inflammatory Disease category for his innovative work on the role of fibroblasts in chronic inflammation. His research, titled:
🧬 “Targeting Fibroblasts in Inflammatory Disease using Engineered T Cells”,
focuses on how tissue-resident fibroblasts contribute to persistent inflammation in diseases such as rheumatoid arthritis (RA) and primary Sjögren’s syndrome (PSS). His team has identified pathogenic fibroblasts in multiple inflammatory conditions and is currently investigating the use of chimeric antigen receptor (CAR) T cells as a novel immunotherapy to specifically target and eliminate these disease-driving cells. This research could lead to a major breakthrough in fibroblast-targeted therapies for inflammatory diseases.
Celebrating Excellence at ACR Convergence 2023
The awards were presented at the ACR Convergence 2023, held at the San Diego Convention Centre, California, from 10–15 November 2023. This flagship annual meeting brings together leading scientists, clinicians, and health professionals from around the world to discuss the latest advancements in arthritis, rheumatic, and musculoskeletal disease research.
Dr Mahony and Dr Kemble’s remarkable achievements reflect the strength of UK-based research in inflammatory diseases and reinforce the University of Birmingham’s role as a leader in rheumatology research. Their work continues to push the boundaries of understanding how inflammation develops and persists, ultimately driving new and more effective treatments for patients.

Listening to Lived Experience: Insights from a JIA Focus Group on Biopsy Procedures
Patient and Public Involvement and Engagement (PPIE) is central to the work of the TRICIA consortium, ensuring that the lived experiences of patients and families directly shape our research priorities and clinical approaches. In paediatric rheumatology, understanding these perspectives is particularly vital, especially when exploring sensitive procedures such as synovial biopsy in children with Juvenile Idiopathic Arthritis (JIA).
On Friday 1st December 2023, a focus group with children and young people diagnosed with JIA and their parents was held at The Exchange, Centenary Square, Birmingham. The session explored the acceptability of biopsy procedures under local anaesthetic with sedation, and gathered views on the timing, communication, and practical aspects of undergoing such procedures.
Key Insights from the Focus Group
1. Anxiety and Pain Management
Participants highlighted concerns around pain, anxiety, and past experiences. They stressed the need for honest, age-appropriate explanations, and reassurance about how pain and anxiety will be managed—particularly the use of sedation and what the procedure would feel like.
2. Tailored Information and Education
Families called for better, clearer educational resources. Videos, visual aids, and real-life patient stories were suggested to help demystify the procedure and build confidence in what to expect.
3. Timing and Practical Considerations
There was a strong preference for biopsies to be performed when the joint is less inflamed or more stable. Concerns were raised about additional hospital visits and balancing procedures with school and family life, highlighting the need for careful planning and flexibility.
4. Supporting Research Participation
Despite concerns, there was a clear willingness to take part in research—especially when families understood how their participation could help shape future treatments and improve care for others with JIA.
5. Communication and Trust
Families emphasised the importance of building rapport with the clinical team and maintaining open, honest conversations. Clear explanations, opportunities to ask questions, and summary documents following discussions all helped to build trust and support informed decision-making.
Taking This Work Forward
The TRICIA consortium recognises that meaningful involvement of patients and families is not optional—it is essential. The insights shared in this focus group will directly inform how we design, deliver, and communicate biopsy procedures as part of our research in childhood arthritis.
We are committed to:
-
Developing age-appropriate educational materials, including videos.
-
Exploring ways to minimise the burden of additional appointments.
-
Ensuring clear, empathetic communication around biopsies.
-
Embedding this feedback into future clinical protocols and research planning.
This focus group is part of our broader effort to make lived experience a core component of TRICIA’s work—ensuring that our studies are designed with patients and families, not just for them.
We are deeply grateful to all the children, young people, and parents who shared their experiences so openly. Their voices are helping to shape a more compassionate and effective approach to paediatric rheumatology research.

Professor Adam Croft Appointed Versus Arthritis Chair of Rheumatology
We are delighted to share that Professor Adam Croft, TRICIA lead and long-standing member of the University of Birmingham’s rheumatology community, has been appointed the new Versus Arthritis Chair of Rheumatology and Head of the Rheumatology Research Group (RRG).
Professor Croft is internationally recognised for his expertise in synovial tissue pathology in inflammatory arthritis and has played a leading role in shaping translational research that connects scientific discovery with real-world impact. Since 2020, he has served as Professor of Translational Rheumatology and continues in his role as Honorary Consultant Rheumatologist at University Hospitals Birmingham (UHB).
“I’m honoured to have been appointed to the Versus Arthritis Chair of Rheumatology at the University, an organisation that has supported my research and that I have long had a relationship with. I look forward to working with researchers in the RRG to shape our research strategy and vision for the next decade, embedding patient views at the heart of our research questions and ensuring Birmingham continues to deliver cutting-edge research that improves the lives and health of people with rheumatic diseases.”
— Professor Adam Croft
A Career Rooted in Birmingham and Built on Translational Impact
Professor Croft began his research journey under the mentorship of Professor Chris Buckley, joining the RRG as part of the NIHR Integrated Academic Clinical Training Pathway. In 2014, he was awarded a prestigious Wellcome Trust Career Development Fellowship, which supported his work on persistent inflammation in chronic immune-mediated inflammatory diseases.
His research has since made a major contribution to the field, including the identification of pathogenic effector fibroblast subsets in inflammatory arthritis. He currently holds a Senior Research Fellowship from the Kennedy Trust for Rheumatology Research.
A Strong Partnership with Versus Arthritis
Professor Croft’s appointment underscores the close partnership between the University of Birmingham and Versus Arthritis, the UK’s leading arthritis charity. The charity supports people with arthritis across the UK, funds world-class research, and campaigns to make arthritis a national priority.
With over 10 million people in the UK affected by arthritis, the impact of the disease is wide-ranging—affecting work, daily life, and independence. As Chair, Professor Croft will play a central role in driving forward research that aims to transform outcomes for people living with rheumatic and musculoskeletal diseases.
Save the Date
📅 Professor Croft will deliver his inaugural lecture on Wednesday 6 March 2024, where he will share his vision for the future of rheumatology research at Birmingham and beyond.

New funding award – Early Detection of Severe Disease in Juvenile Idiopathic Arthritis
Professor Adam Croft has been awarded £392,004.48 by Versus Arthritis for the project ‘Early Detection of Severe Disease in Juvenile Idiopathic Arthritis’. Starting on 1st August 2023 and running for three years, this funding aims to advance our understanding and treatment of Juvenile Idiopathic Arthritis (JIA).
As part of the Versus Arthritis funded Multiomic Analysis of Paediatric Gut and Joint Inflammation (MAPJAG) study, Prof Adam Croft pioneered the application of a safe, well-tolerated technique for minimally invasive ultrasound-guided synovial tissue biopsies in children and young people with inflammatory arthritis. In this project, the research team defined the cellularity of the synovial tissue at single-cell (sc) resolution using scRNA-sequencing of digested tissue from individuals with an actively inflamed joint. This new funding will allow analysis to extend to matched blood and synovial fluid samples and fund complementary spatial analysis of matched tissue.
This study is embedded into the TRICIA network and will draw on the intellectual infrastructure across four academic institutions; Oxford, UCL, UoB, and Manchester
European Workshop for Rheumatology Research

Consortium Launch
Funded by a UKRI partnership grant, TRICIA is a collaborative network across four academic institutions: Manchester, University College London, Birmingham and Oxford and has collective expertise in epidemiology, pathophysiology, data science and bioinformatics. Its objective is to build capacity within UK paediatric rheumatology to perform synovial tissue biopsy studies to improve treatments for Juvenile Idiopathic Arthritis (JIA) through precision pathology research.
This collaboration will allow for larger-scale synovial tissue research studies in the future, enabling the identification of new pathways, signatures, targets, and biomarkers. The ultimate goal is to improve the lives of those affected by JIA